Creatinine Levels
As a nurse, you should always be aware of a patient's creatinine levels. This is normally drawn as part of a comprehensive or basic metabolic panel. Why does this lab value matter so much? This can tell you a great deal about how the kidneys are functioning.
What is Creatinine?
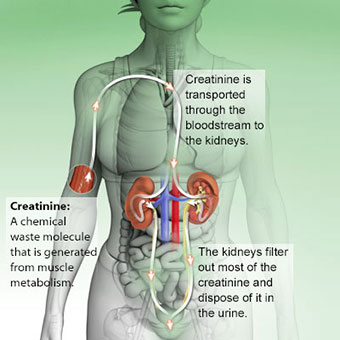
Creatine (not to be confused with creatinine) is a waste product from the breakdown of muscles during metabolism. Creatinine is produced from creatine. Creatinine travels to the kidneys through the bloodstream and is excreted in urine.
Why Does This Matter?
The creatinine level of a patient is a reliable way to evaluate their kidney function. The normal range for creatinine levels is 0.62 - 1.66 mg/dL. Elevated levels can indicate there is either acute or chronic kidney disease.
One of the main purposes of the kidneys is to filter out the things that your body does not need. The creatinine level is a guide for how well the kidneys are actually filtering the patient's blood. If they are filtering out the creatinine (and hopefully everything else) the way they should be then the body continues to function normally. If the creatinine levels become too elevated, it is showing that the kidneys are not doing their job of filtering. To fix this, the patient may require dialysis to assist with filtration.
Nursing Tip: When I am caring for a patient who is in need of any electrolyte replacement, I always make sure to know the patient's creatinine and average urine output prior to calling the doctor. They will definitely want to know how their kidney's are functioning prior to giving any kind of electrolyte replacement.
Patient Experience
I have cared for many patients with end stage renal disease (ESRD). Much of the time they have a co-morbidity of either type two diabetes or hypertension which led to their kidney problems.
A typical report on an ESRD patient that might be seen in the ICU looks something like this: The patient is a 65-year-old male admitted with fluid overload. He gets hemodialysis (HD) on Monday, Wednesday, and Friday each week. He wasn't feeling well and missed his last two HD sessions. His creatinine was 8.89 mg/dL and his potassium was 6.0 on admit. (The kidneys are essentially "broken" so they don't filter out the creatinine or electrolytes (including potassium) the way that they should.) He was very fluid overloaded and could hardly breathe. He was on 10L simple mask, tachypneic (fast respiratory rate), and tachycardic (fast heart rate). The patient received emergent HD where they removed 2.5 liters of fluid. He's now on 5 liters of oxygen via nasal cannula with clear lung sounds. After HD, his creatinine was 6.6 mg/dL and his potassium came down to 4.5.
It is always interesting to me to look at the creatinine level and see how it changes. You expect it to rise up leading to HD and then decrease with the next lab draw post-HD. The creatinine can be an excellent measurement for the recovering kidney transplant patient as well. A patient's creatinine is usually extremely elevated (I've seen as high as 12!) prior to transplant. It's amazing to watch the creatinine drop by multiple points with each blood draw post-operatively. You get to see the new kidney in action!
Other relevant articles include:
Resources