The following guest article was written by Jessica Hegg from ViveHealth.com. She is a wealth of knowledge on managing bedsores and how we, as nurses, can help our patients.
Bedsore Management
Bedsores, also known as pressure sores or pressure ulcers, require vigilant attention and treatment from stage I, especially for ICU patients and patients with mobility issues which limit them to the bed or a recliner.
How Do Bedsores Form?
Overtime, when a weakened body is left in the same position (i.e. lying in bed without being moved), bony protrusions on the body (typically on the elbows, shoulder blades, tailbone, hips, and even the heels) press down on internal tissues. This cuts off blood flow and can lead to tissue breakdown as well as the maceration and breakdown of the epidermis. Cracked, open wounds degenerating from the outside and the inside can quickly become infected, degrade, or worse.
What Does A Bedsore Look Like?
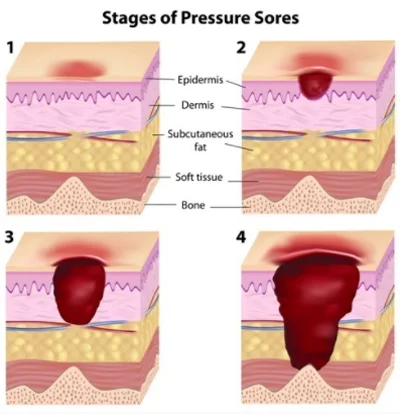
Initially evaluated as simple redness or discoloration of the skin, a stage I bedsore should be monitored closely and as much as possible, prevented from progressing further. If you can lightly press the reddened area and it blanches (loses color briefly then flushes red again), that is a good sign that there is no tissue damage yet.
A stage II bedsore will include broken skin on the reddened area and what looks like the start of an ulcer. It will be painful and tender to the patient. A stage III bedsore is diagnosed when a crater begins to form as more and more layers of tissue are damaged. And a stage IV bedsore involves tissue breakdown all the way down to layers of muscle and bone, putting patients at a greatest risk for infection and permanent damage.
How Do I Prevent Bedsore Progression?
To combat bedsore progression at the slightest hint of redness and discoloration on a bonier part of the body, a patient must have their body weight shifted regularly (at least every 2 to 3 hours). This can be done simply by stuffing pillows under one side or the other of the patient’s back and bottom, to where they are comfortable but also not resting on problem areas. A pillow to prop legs up and float the heels in the air is best practice as well to prevent rubbing, irritation, and potential skin breakdown on the back of the feet.
Additional items which help might include an alternating air pressure mattress (or specialty mattress), which requires a written order from the overseeing doctor or wound care team. For home health patients, air pressure mattresses, memory foam and gel mattress toppers, also provide bedsore prevention by more evenly distributing body weight when lying and sitting down.
Additional factors which exacerbate bedsores include:
Poor diet that lacks tissue building nutrients and vitamins (like zinc, protein, calcium, and Vitamin C)
Incontinence (the constant moistness of vulnerable areas like the tailbone, plus bacteria from urine and fecal matter)
Poor circulation associated with smoking, diabetes, and other circulatory diseases
Being underweight to where a patient’s body lacks vital cushioning from muscles and tissue
Older age as elderly patient’s skin will lack the elasticity and strength to prevent breakdown as much as a younger one
Cognitive impairment wherein a patient in a coma or with brain damage may not be able to convey pain or sensation from a bedsore
How Are Bedsores Treated?
In addition to shifting weight, boosting circulation, and proactively strengthening skin with diet and incontinence management, bedsores can be treated with dressings and topical applications like with other wounds, say from surgery or injury.
Barrier creams play a vital role in staving off bedsore progression. They can be applied to closed stage I bedsores to keep moisture and potential contaminants out. Ointments, gels, and creams (like MediHoney, CoronaCream, and EPC with zinc-oxide) serve this barrier role and will typically be recommended by a wound care specialist if needed.
Wound dressings for stage II - IV bedsores include a variety of sizes, types, and strengths like are found on the wound dressing page. Dressings might include silicone padding with an adhesive barrier (like with Mepilex), hydrophilic foam dressing (i.e. HydraFoam), hydrocolloid dressing (i.e. DermaFilm HD), and alginate dressings (they contain calcium and sodium fibers derived from seaweed and can absorb fluids to promote healing on late-stage wounds).
Bottom Line
No matter the setting - home, hospital, or nursing home, bedsores should always be taken very seriously. For many with chronic disease or mobility issues, a bedsore might not seem like a priority compared to other health conditions; however, their nature to progress quickly and lead to infection definitely make them a wound to keep an eye on.
Author Biography
Jessica Hegg is the content manager at ViveHealth.com. Avid gym-rat and nutrition enthusiast, she’s interested in all things related to staying active and living healthy lifestyle. Through her writing she works to share valuable information aimed at overcoming obstacles and improving the quality of life for others.
Other relevant articles include: